Midwife Problems, and Solutions, part 4This is part four of a series on midwifery in Sweden and the United States. To read part one click here, part two click here, part three click here.
4 Comments
Midwife Problems, and Solutions, Part 3This is part three of a series on midwifery in Sweden and the United States. To read part one, click here, to read part two, click here.
And during all this uncertainty, Johan van Hoorn was hoping someone would listen to him and his talk of jordegumman. Van Hoorn had studied medicine in the Netherlands and Paris, and had returned to Sweden to practice medicine and ended up spreading his gospel of training the midwife.
In Old English, midwife means with-woman, in Swedish jordemor (the jord comes from the Old Norse word for child or offspring) and barnmorska both mean child-mother. In Sweden at the end of the 1600s, most were untrained women known as jordegummor. Van Hoorn wanted to elevate their status, he wanted to make them barnmorskor. First, he put out the textbook called Then Swenske wäl-öfwade Jord-Gumman in 1697. In 1715, he published The Twenne Gudfruchtige I sitt kall trogne Och therföre af Gudi väl belönte Jordegummor Siphra och Pua, a textbook of questions and answers for midwives. Midwife Problems, and Solutions, Part 2This is part 2 of a series on the history of midwifery in the U.S. and Sweden. Click here to read part 1.
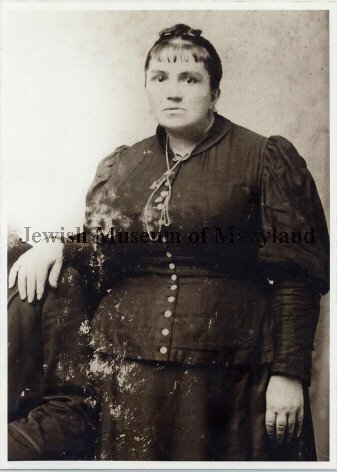
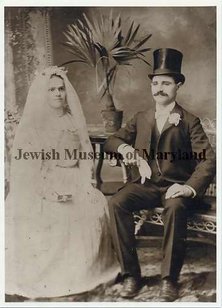
In Baltimore city, over 150 midwives delivered over 4,000 babies a year, and in every city and town in the U.S., you could find a woman delivering a baby, calling herself a midwife. But just like there were no regulations for doctors, there were no regulations for midwives. Why didn't the U.S. regulate the medical profession? And what did that mean for the health and safety of babies and mothers?
(Hey! I'm trying something new here, with a series of short, interconnected posts based on research and archives I visited in the fall of 2015, relating to Swedish midwifery and comparing it to the U.S. Let me know what you think in the contact section.) Hanna Karlen arrived in Boston on October 11, 1901 with four pieces of luggage. She was 36, traveling alone. On the ship's manifest, Karlen called herself a nurse, a statement that wasn't totally accurate.
It is really so amazing that in modern documents like this, Frau Conti is recognized as the President of the ICM, yet there is no mention of the backdrop of what was going on in 1936 in Berlin when they held this Congress, and the terrible implications of her politics and practices.
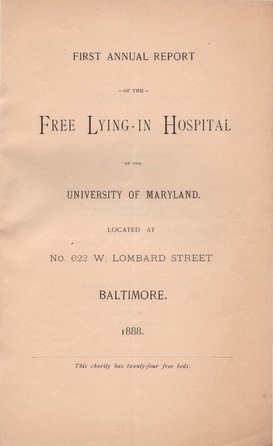
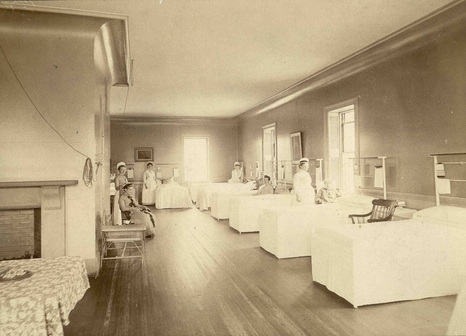
The year that the Lying-In hospital opened, the only other hospitals for women in Baltimore were the Maryland Woman's Hospital (at 112 E. Saratoga St.) and the Maternite Lying-In-Asylum at 113 E. Lombard St., both associated with the College of Physicians and Surgeons. Part of the reason that medical schools opened hospitals was so that their students could learn by seeing patients, not just sitting in a classroom. Intern years and residencies were not officially part of the medical school curriculum yet. The Lying-In Hospital gave the University of Maryland, where Dr. Miltenberger and Dr. Neale were both graduates of and professors at, a perfect opportunity to help and teach. "The large proportion of needy poor and unfortunates in every large city calls loudly for aid for simple charity's sake, while the benefits to the community, both present and future, from an institution where practical instruction at the bed-side could be afforded to advanced students, are self-evident." - First Annual Report p. 8 The Lying-In Hospital came at the advent of the new era of hospital. The wards were large, with high ceilings and white-washed walls. The beds were made of painted iron. The simple construction made them easy to clean. On top of the bed frame there were wire-spring mattresses, a relatively new invention that was much cleaner and hygienic than stuffed mattresses. Although they didn't have running water in the wards (Baltimore would not have a city-wide sewer system for another 24 years), polished-surface basin and pitcher were used for cleaning patients.
Another distinct feature was that both white and black people were attended to in the hospital. Johns Hopkins would become famous for serving all races of poor people a few years later, but the Lying-In Hospital was already doing it. However, the report does make a specific point that the two wards are separate from one another. In their first seven months of operation, the hospital saw 62 women, 57 of whom gave birth. Two women died, most likely a result of postpartum hemorrhage since no cases of septicemia were reported. Four out of fifty-eight children died, a relatively low rate compared to national infant mortality, which continued to be as high as twenty percent in some areas into the 21st century. I'll end with my favorite quote from the 1st report: "All malt liquors, wines, spirits, etc., brought to the house shall be placed in charge of the Matron, and used only by order of the attending physicians." |
Come in, the stacks are open.Away from prying eyes, damaging light, and pilfering hands, the most special collections are kept in closed stacks. You need an appointment to view the objects, letters, and books that open a door to the past. Archives
April 2023
Categories
All
|







 RSS Feed
RSS Feed